Granulomas See DX Path for details of the conditions below
If you look at the slide and you see in the dermis collections of epithelioid histiocytes plus or minus surrounding lymphocytes or giant cells or neutrophils in the centre of these lesions, then you have granulomas.
If you look at the slide and you see in the dermis collections of epithelioid histiocytes plus or minus surrounding lymphocytes or giant cells or neutrophils in the centre of these lesions, then you have granulomas.
Granulomas are sub-classified into about four types. They can be tuberculoid, sarcoidal, pallisading or infectious.
Various diseases present as different types of granulomas.
The sarcoidal granuloma is sometimes called the naked granuloma because basically you just have a collection of histiocytes without any surrounding lymphocytes or neutrophils.
In a tuberculoid granuloma you will have histiocytes but you will also have some central caseous necrosis. In the pallisading granuloma you will find that the cells are surrounding denatured collagen and it goes under the name of necrobiosis or sometimes there is mucin or foreign body material at the centre of a pallisading granuloma.
A suppurative granuloma has centrally numerous neutrophils and they are part of an infected abscess.
Various diseases present as different types of granulomas.
The sarcoidal granuloma is sometimes called the naked granuloma because basically you just have a collection of histiocytes without any surrounding lymphocytes or neutrophils.
In a tuberculoid granuloma you will have histiocytes but you will also have some central caseous necrosis. In the pallisading granuloma you will find that the cells are surrounding denatured collagen and it goes under the name of necrobiosis or sometimes there is mucin or foreign body material at the centre of a pallisading granuloma.
A suppurative granuloma has centrally numerous neutrophils and they are part of an infected abscess.
The granuloma is the body's immune attempt at isolating this infective process. The common granulomatous diseases we see will be sarcoidosis, granuloma annulare, actinic granuloma, granulomatous rosacea, necrobiosis lipoidica, tuberculosis of the skin and leprosy. The other condition we have to watch out for is the deep fungal infection which will have an infective granuloma.
GRANULOMAS IN THE DERMIS
(Use the GlobalSkinAtlas Page link at the top of this website to access Clinical Images of some of these cases.)
(Use the GlobalSkinAtlas Page link at the top of this website to access Clinical Images of some of these cases.)
If you look at the slide and you see in the dermis collections of epithelioid histiocytes plus or minus surrounding lymphocytes or giant cells or neutrophils in the centre of these lesions, then you have granulomas.
Granulomas are sub-classified into about four types. They can be tuberculoid, sarcoidal, pallisading or infectious (Suppurative). Various diseases present as different types of granulomas. Foreign body material can cause any type of granuloma but usually it is sarcoidal. The sarcoidal granuloma is sometimes called the naked granuloma because basically you just have a collection of histiocytes without any surrounding lymphocytes or neutrophils. In a tuberculoid granuloma you will have histiocytes but you will also have some central caseous necrosis. In the pallisading granuloma you will find that the cells are surrounding denatured collagen which goes under the name ofnecrobiosis or sometimes there is mucin or foreign body material at the centre of a pallisading granuloma. A suppurative granuloma has centrally numerous neutrophils and they are part of an infected abscess. Mind you the commonest cause of a suppurative granuloma is a ruptured follicle or cyst.
The granuloma is the body's immune attempt at isolating this infective or inflammatory process. The common granulomatous diseases we see will be ruptured follicular cyst, sarcoidosis, granuloma annulare, actinic granuloma, necrobiosis lipoidica, tuberculosis of the skin and leprosy. The other condition we have to watch out for is the deep fungal infection which will have an infective granuloma. Let's look at the histopathology of each of these conditions in turn.
Granuloma Annulare (See Clinical Images)
This shows a pallisading or interstitial pattern where you have histiocytes, lymphocytes and some mucin in between collagen fibres in the dermis and these collagen fibres are necrobiotic. Sometimes this is described as both the interstitial and the pallisading pattern. The infiltrating type is the interstitial one and the pallisading pattern is where you have a central core of collagen with histiocytes surrounding it. Mucin is seen in granuloma annulare but it isn't seen in necrobiosis lipoidica, but sometimes you need a colloidal iron stain to show up the mucin. Granulomas may also have giant cells associated with them and the ones that are classically described are the Toton giant cell where the nuclei are in a circle; the Langerhans giant cell where the nuclei are peripherally placed and in a horseshoe shaped pattern and the foreign body giant cell where there is a diffuse arrangement of the nuclei in the cell. A deep form of granuloma annulare in which the histiocytes pallisade around fibrin rather than mucin can be indistinguishable from a rheumatoid nodule.
It is also useful to compare and contrast granuloma annulare with necrobiosis lipoidica. Essentially in granuloma annulare the granulomas are focal and patchy whereas necrobiosis lipoidica is diffuse and often involves the full thickness of the dermis down to and including the fat layer. The granuloma is pallisading or interstitial in granuloma annulare but in necrobiosis lipoidica you can have a layered or sandwich granuloma. Mucin present in granuloma annulare but not in necrobiosis lipoidica. Plasma cells are common though in necrobiosis lipoidica but are rare in granuloma annulare and cholesterol clefts can sometimes be seen in some old lesions of necrobiosis lipoidica but not in granuloma annulare.
A variant of granuloma annulare that should be recognised is perforating GA. Typically these lesions occur on the back of the hands or feet and the papules have a central crust or small umbilicated area where the abnormal collagenous material is being extruded through the overlying epidermis.
See this Clinical Variant in GlobalSkinAtlas
A variant of granuloma annulare that should be recognised is perforating GA. Typically these lesions occur on the back of the hands or feet and the papules have a central crust or small umbilicated area where the abnormal collagenous material is being extruded through the overlying epidermis.
See this Clinical Variant in GlobalSkinAtlas
Actinic Granuloma
This was first described by an Australian, John O'Brien and it is typically seen on sun exposed areas particularly the neck. In these lesions there is a spreading edge with loss of elastic fibres in between so that if a special stain is done for elastic fibres they won't be there. Actinic granuloma shows a similar pallisading picture as in granuloma annulare but there is no mucin and it has this central loss of elastic tissue. Biopsies should be taken from the edge and centre of these lesions or do an ellipse across the edge from normal skin to granulomas to loss of elastic tissue.
Necrobiosis lipoidica (See Clinical Images)
The changes in the collagen are necrobiotic changes extending quite deeply into the reticular dermis in this condition. There is often a layered infiltrate of lymphocytes and histiocytes in between the damaged collagen. Mucin isn't usually seen. Plasma cells may be seen particularly in the deep dermis and the degenerate necrobiotic collagen is very prominent. It is probably more prominent in necrobiosis lipoidica than it is in granuloma annulare. Many patients with necrobiosis lipoidica have or will develop diabetes mellitus. The term necrobiosis refers to alteration in the dermal connective tissue. There is loss of cellular definition, the area stains quite palely and as we said before there is an absence of mucin. A deep incisional biopsy is best with primary closure as otherwise healing can be slow.
Necrobiotic Xanthogranuloma
Though the terminology may seem similar to necrobiosis lipoidica, the condition is potentially more serious. Again you have broad zones of granuloma formation, may you may also see Toton giant cells and Langerhans giant cells. In older lesions cholesterol clefts can also be seen and there may be plasma cells and even lymphoid follicles. Necrobiotic Xanthogranuloma typically involves the face and the periocular skin. It may also involve the scalp. The clinical lesions are yellowish with prominent vessels and the patients usually have an abnormal light chain gamma globulin circulating in the blood. Usually it is an IgG kappa light chain and they have a paraproteinaemia. Note that giant cells are more common in Necrobiotic xanthogranuloma than in necrobiosis lipoidica.
Juvenile Xanthogranulomas (See Clinical Images) are not commonly biopsied. They may occur in young children as the name suggests, but xanthogranulomas can also occur at any age. The initial lesions look red and may be confused because of their rapid growth with a Spitz naevus, but over time they become yellow or yellow/orange. Histologically there are a lot of histiocytes in the papillary and reticular dermis and Tuton giant cells may be seen.
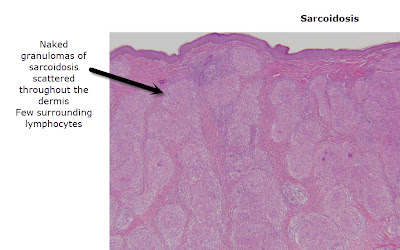
Sarcoidosis (See Clinical Images)
Sarcoidal granulomas are regarded as naked granulomasin that there is just a collection of epithelioid histiocytes. There may be a thin rim of lymphocytes but they don't disperse through the granuloma. Epithelioid means that the histiocytes look like epidermal keratinocytes. No necrosis or necrobiosis is usually seen in these lesions. Sarcoidosis is a great mimic clinically so it may present as a variety of skin diseases and have lung or cardiac problems, or rarely even hypercalcaemia. Sometimes cutaneous lesions are seen in about 25% of patients who don't show any signs of systemic sarcoidosis. It is usually seen histologically as a diagnosis of exclusion in that infectious causes should be looked at with special stains and also polarising microscopy should be used to see that thisisn't a sarcoidal reaction to a retained foreign body. Silica material can typically cause this as can Zirconium and even mercury. Other conditions that can show naked granulomas include Crohn's disease, the Melkersson Rosenthal syndrome with granulomatous cheilitis, silica granulomas and granulomatous rosacea.
These are sarcoidal reactions at the site of a graze injury. The patient may or may not have systemic sarcoidosis
These are sarcoidal reactions at the site of a graze injury. The patient may or may not have systemic sarcoidosis
Granulomatous rosacea is one of the unusual variants of rosacea. The granulomas are typically tuberculoid rather than sarcoidal, but there is a degree of overlap. Usually in granulomatous rosacea there are also follicular pustules and telangictasia. The variant perioral dermatitis has a histopathology just the same as rosacea. Another condition that is similar is acne agminata or lupus milliaris disseminatus faceii. These lesions are firm brownish papules usually found on the forehead. They will show a pallisading granuloma but in the centre is a large area of caseous necrosis and hence they look like TB. However when you do special stains or PCR there is no evidence of tubuculoid organisms.
Rarely drug reactions can cause an interstitial granulomatous pattern.
In tuberculoid granulomas they are often fairly poorly formed granulomas. You often get central caseous necrosis but not always. There is usually around the granuloma a large number of lymphocytes and plasma cells. You may occasionally get some multi-nuclear giant cells with asteroid and schaumann bodies.
Leprosy also gives a epithelioid granuloma of the tuberculoid type. There is usually a prominent rim of lymphocytes with a bit of central ccasseation. The granulomas are particularly localised around large named nerves and the picture differs a bit depending on the degree of immunogenicity of the patient. If there is a fair level of immunity then tuberculoid leprosy will occur with granulomas but few organisms. If there isn't then you will tend to have lepromatous leprosy in which there are a multitude of organisms and the granulomas aren't as well formed.
Foreign body granulomas
These are due to material such as tattoo pigment or quartz or glass or even beryllium. Usually this material is birofringent and polarised to light, but other foreign bodies even sea urchin spines can give a similar picture. Non-birefringent material includes chromium seen in deodorants and some tattoo pigments, the commonest of which is red tattoo containing mercury or cinnabar.
In summary if there is a dermal granulomatous pattern look to see if it is a sarcoidal or tuberculoid or pallisading granuloma or an infective one. Look to see if you just have epithelioid histiocytes or a type of giant cell that is there. See if there is any central caseous necrosis. See if there are lymphocytes or plasma cells surrounding the granuloma. Look to see if there is any altered collagen . Ask for special stains to look for acid and alcohol fast bacilli. The Wade Fite stain is better than the Ziel Neilsen. Always do polarising microscopy to see if there is any birefringence indicating a foreign body.
Infective Granulomas - Deep fungal infections- Sporotrichosis
Here you may as well as seeing a granulomatous process in the dermis see pseudo epitheliomatous hyperplasia. You get a suppurative granuloma and when special stains are done you may see the fungal spores of sporotrichosis – these are usually cigar shaped. Chromoblastomycosis can give a similar picture but here you may get clusters of brown spores when you use the appropriate stain which are sometimes known as "copper pennies".
Granulomas are sometimes seen when you have a ruptured cyst or follicle and these are generally localised around hair follicles or cystic structures. They are probably the commonest granulomas biopsied in clinical practice.
The condition interstitial granulomatous dermatitiswill histologically show pallisading and neutrophilic granulomatous dermatitis. The lesions are often skin coloured papules with an umbilicated or crusted surface. Patients with these lesions can often have autoimmune diseases such as rheumatoid arthritis or lupus or may even have lymphomas, so this interstitial granulomatous dermatitis is important but it can also be caused by certain drugs, particularly the calcium channel blockers, beta blockers, ACE inhibitors and even some antihistamines. The histological picture of the interstitial granulomatous drug reaction is similar to granuloma annulare with a busy dermis. There may be epidermotropism as well and this is what makes you think there may be an underlying lymphoma. It can also be a lichenoid reaction with vacuolar changes as well. This is more suggestive of a drug cause. View this link for more details
The last and very rare condition to mention isgranulomatous mycosis fungoides or granulomatous slack skin disease. Here you have a granulomatous infiltrate in the dermis which also destroys elastic fibres similar to actinic granuloma. The diagnosis is made on the basis of the atypical lymphocytes that form these granulomas. View this link for more details.











No comments:
Post a Comment
Note: Only a member of this blog may post a comment.